Working in Teams
Teamwork and Patient Safety
Healthcare systems still suffer, as do patients, from an unacceptable level of adverse events (harm from care not from disease) which at least half can be prevented through system change. Breakdown in teamwork and communication is a constant root cause in most analyses of these adverse events. As a result, working in teams has evolved as an essential competency for all healthcare professions to acquire through their life-long education and training.
Teams
True teams are composed of at least two individuals working interdependently towards shared goals / objectives and who create time to reflect on their progress towards their achievement. In team-based healthcare, team members also work collaboratively with patients and their families in establishing shared goals / objectives that ensure safe quality care.
Muti-Team Systems
Care is interprofessional and involves work of multiple care teams. Patients along their care pathway encounter several teams of various professions each with their own roles and responsibilities. Healthcare is a multi-team system and attributing patient outcomes to a single care team is simplistic and ignores this complexity. In order to ensure safe integrated care, teams have to develop not only their intra-team skills but also their inter-team collaboration skills.
Culture and Climate
It is important to have an organizational culture and local working climates that encourages staff to work in teams and share their experiences and concerns.
Positive organizational cultures are characterized by:
-
- Clear missions;
- Consistent policies;
- Engaged staff;
- Capacity to adapt and learn.
Positive working climates are characterized by:
-
- Commitment to team approach in providing care;
- Respecting and valuing contributions of team members regardless of profession or seniority;
- Mutual accountability for team performance;
- Acknowledgement of team member fallibility regardless of profession or seniority.
Team Effectiveness
Team effectiveness encompasses a set of different, but related, dimensions and therefore can mean different things to different people.
However, team effectiveness is usually related to the following:
-
- Team performance: the extent to which the team is successful in achieving its goals, especially those that contribute to the accomplishment of the organization mission;
- Team member well-being: referring to team members physical and mental health, professional development and growth;
- Team viability: the likelihood the team will continue to work together and function effectively;
- Team innovation: the extent to which the team develops and implements new and improved processes, products, and procedures;
- Inter-team cooperation: capacity of the team in working with other teams within and without the organization.
Team Building
It is important when building teams that their composition reflects the multidisciplinary nature of healthcare and that team members from each profession respect and value the role and contribution of team members from other professions in order to ensure collaborative practice.
Building effective teams require the establishment of the following elements:
-
- Team goals with measurable outcomes that are aligned with the organization mission;
- Availability of clinical and administrative systems that support team members in the achievement of team goals;
- Division of labour among team members including defining team tasks and assignment of roles;
- Team members training in their roles and cross-training to ensure continuity of care in case of absences or increase workload;
- Communication structures (meetings, routine communication, minute-to-minute communication) and processes (reflection, feedback, conflict resolution).
Team-Based Health Care
Team-based health care (TBC) is the provision of health services to individuals, families, and/or their communities by at least two health providers who work collaboratively with patients and their caregivers, to the extent preferred by each patient, to accomplish shared goals within and across settings to achieve coordinated, high-quality care.
Values of TBC
The following 5 personal values are important for individuals to function well within healthcare teams:
Honesty. Honesty and transparency of aims, decisions, uncertainty, and mistakes are critical to continued improvement and for maintaining the mutual trust necessary for a high-functioning team.
Discipline. Team members carry out their roles and responsibilities with discipline, even when it seems inconvenient.
Creativity. Team members are innovative in tackling new or emerging problems. They see errors and unanticipated bad outcomes as potential opportunities to learn and improve.
Humility. Team members recognize that they are human and will make mistakes regardless of profession and seniority. Hence, they rely on each other to help recognize and avert failures.
Curiosity. Team members are dedicated to reflecting upon the lessons learned in the course of their daily activities and using those insights for continuous improvement of the functioning of the team.
Principles of TBC
Each health care team is unique but the following 5 core principles are important for all healthcare teams to follow:
Shared goals. The team, including the patient (where appropriate) and carers, works to establish shared goals that reflect patient and carer priorities, that can be clearly articulated and supported by all team members.
Clear roles. There are clear expectations for each team member’s functions, responsibilities, and accountabilities, which optimize the team’s efficiency thereby accomplishing more than the sum of its parts.
Mutual trust. Team members earn each others’ trust, creating strong norms of reciprocity and greater opportunities for shared achievement.
Effective communication. The team prioritizes and continuously refines its communication skills. It has consistent channels for candid and complete communication, which are accessed and used by all team members across all settings.
Measurable processes and outcomes. The team agrees on and implements timely feedback on successes and failures in relation to teamwork and achievement of goals. These are used to track and improve performance immediately and over time.
Team Processes
Teams have different tasks to do and one should differentiate between taskwork and teamwork. For example, a surgical team has the task to perform surgery on patients while an ICU team has the task to care for patients on ventilators. However, they both have to know how to work together as a team to ensure the delivery of desired outcomes. In other words, taskwork represents the functional activities that teams must accomplish, while teamwork represents the collaborative processes that help team members work together. Team processes are used to direct, align, and monitor taskwork.
Teams perform their tasks through cycles of activity characterized by periods of action and transition of variable time depending on the nature of the task and the strategy chosen to accomplish it. Action phases are periods of time when teams are engaged in acts that contribute directly to goal accomplishment (i.e. taskwork). In contrast, transition phases are periods of time when teams focus primarily on planning and evaluating their activities to guide or adapt their future activities.
The nature of teamwork (team processes) changes as teams move from phase to phase with some that are common to both transition and action phases.
Transition Phase Processes
Transition phase processes aim at planning future action and reflecting on past activities. They include mission analysis, goal specification, and strategy formulation. Team members have to explicitly know their mission and ensure it is aligned with their organization’s mission, culture and resources. In doing so, team members are expected to discuss their goals and how they intend to achieve them (strategy). Similarly, team members are expected to explicitly reflect on their past activity to know what went well and what went not so well and what are the lessons learnt and how to be more effective as a team during future activity.
Transition phase process are sometimes needed during action phases (see Figure) when things are not working well and the team needs to modify their goal or adapt their strategy in response to unexpected events.
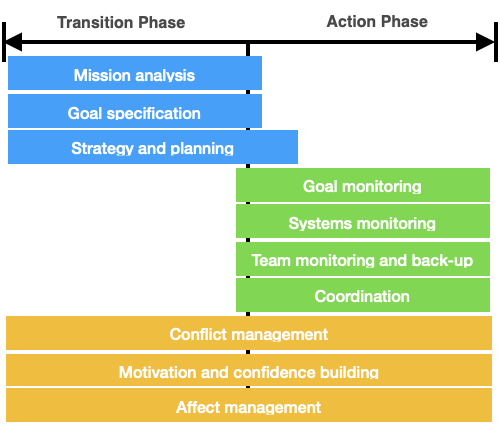
Action Phase Processes
Action phase processes aim at ensuring the effective and safe accomplishment of tasks. These processes include monitoring goal achievement through regular feedback as a form of self-regulation and performance control. Monitoring team resources and working environment using available information ensures proper situation awareness and timely adaptation. Monitoring team members’ performance safeguards task-related support when necessary and gives the chance for team members to ask for help when needed. Coordination of activities by team leadership ensures their proper and timely sequencing. Effective communication with timely feedback guards against poor coordination and process loss.
Interpersonal Processes
Interpersonal processes occur during both phases and aim at creating healthy relations between team members and at resolving any emergent conflict between them. Task or relationship conflicts should be resolved through agreed-upon proactive and reactive win-win approaches that preserve both team performance and relations. Team members’ motivation towards achieving team mission and goals should be first protected by eliminating work dissatisfaction conditions then followed by creating conditions that enhance work satisfaction. Affect management involves regulating team emotions during mission accomplishment through effective perception and management of in self and in others emotions.
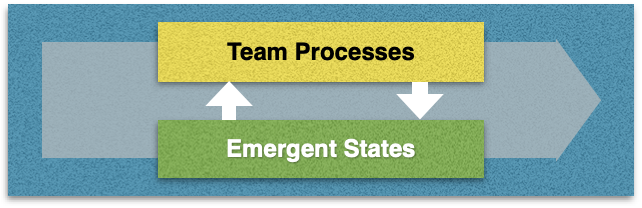
Emergent States
Emergent states are team properties that emerge from team experiences (interactions) and they describe team members' attitudes and feelings towards the team. Team states are dynamic in nature and vary as a function of team inputs, processes, and outcomes. Shared mental models, psychological safety, team cohesion and mutual trust are examples of team emergent states.
Team emergent states can be considered proximal outcomes of teamwork that affect interpersonal team relations and performance. In this context they also act as inputs to subsequent team processes.
Processes and states are not always easily distinguishable. An effective way to assess whether we are dealing with a process or a state is to look at the words we use to describe the issue. If we are using action verbs, most likely we are talking about team processes. In contrast, if we are using adjectives, we are probably dealing with team states.
Shared Mental Models
A mental model is one’s understanding of the surrounding circumstances. Shared mental models evolve when team members have the same understanding. The information or knowledge that is shared among team members is either taskwork or teamwork related. It is important to ensure that what is shared among team members is similar, resembles reality and is responsive to evolving circumstances.
Psychological Safety
Psychological safety is the belief that one will not be punished or humiliated for speaking up with ideas, questions, concerns, or mistakes. In teams, it refers to team members believing that they can take risks without being shamed by other team members. In other words, psychological safety means that teams members feel included and respected, have opportunities to learn, can contribute to teamwork and can challenge the status quo without negative consequences.
Team cohesion
Team cohesiveness is defined as the extent to which members are attracted to the team and motivated to remain in it. Task cohesiveness is the extent to which team members are motivated towards achieving team mission and goals. Similarly, social cohesiveness refers to team members motivation to develop and maintain social relationships within the team.
Mutual Trust
Mutual trust is established when team members believe in the reliability, integrity, and trustworthiness of one another, and openly rely on each other because of this belief.
Reading Material
Teamwork and Patient Safety
-
- Mitchell P, et al. Core principles and values of effective team-based health care. IOM. 2012.
- Weaver SJ, et al. Improving patient safety and care quality. A multiteam system perspective. Research on Managing Groups and Teams. 2014;16:35-60.
- West MA. Effective teamwork.Practical lessons from organizational research. Wiley-Blackwell. 2012.
- Grumbach K, et al. Can healthcare teams improve primary care practice. JAMA. 2004;29:1246-51.
Team Processes and Emergent States
-
- Marks MA, et al. A temporally based framework and taxonomy for team processes. Acad Manage Rev. 200;26:356-376.
- McComb S and Simpson V. The concept of shared mental models in healthcare collaboration. J Adv Nurs. 2014;70:1478-88.
- Clark TR. The 4 stages of psychological safety. Berrett-Koehler Publishers, Inc. Oakland. 2020.
- Barsade SG and Gibson DE.Why does affect matter in organizations? Academy of Management Perspectives. 2007;21:36-59.